We’ve all heard people call stress “the silent killer”. Frankly, it’s a bit of a tired cliché.
However, taking into consideration the monumental level of disarray the world is in these days, what were once silly platitudes about stress and health have taken on an air of immediacy that asks us to take another look at the science, especially when it comes to how stress impacts the immune system.
Have you ever known anyone who has fallen apart after going through an incredibly stressful period, such as a divorce or losing a loved one? These aren’t coincidences.
Although stress is clearly not always the sole cause of disease, it’s something that researchers have found can powerfully catalyze the progression of many conditions by driving up inflammation and weakening the immune system.
And this isn’t just spiritual people like Oprah, Eckhart Tolle, and Deepak Chopra saying this. There are researchers around the world uncovering the various mechanisms by which chronic stress can deplete our immune systems and leave us vulnerable to chronic inflammatory illness.
For example, the authors of this study on stress-induced immune dysregulation say:
“Stress-related immune alterations can…enhance susceptibility to infectious agents and influence the severity of infectious disease, diminish the strength of immune responses to vaccines, reactivate latent viruses, and slow wound healing.”
Countless studies have been performed showing the relationship between stress, mood, and immunity. Researchers have associated altered immune function with loneliness, depression, and even social defeat (although that study was unfortunately done on rats, if you can imagine that).
In fact, the connection between the immune system, stress, inflammation, and mood is so supported by research that there’s an entire book on the topic, titled “Cytokines and Depression: How Your Immune System Causes Depression”.
Integrative medicine psychiatrist Dr. Kelly Brogan is one of the more well-known proponents of this new model of depression, which shows that neurotransmitters like Serotonin and Dopamine can be reduced by inflammatory cytokines generated by the immune system.
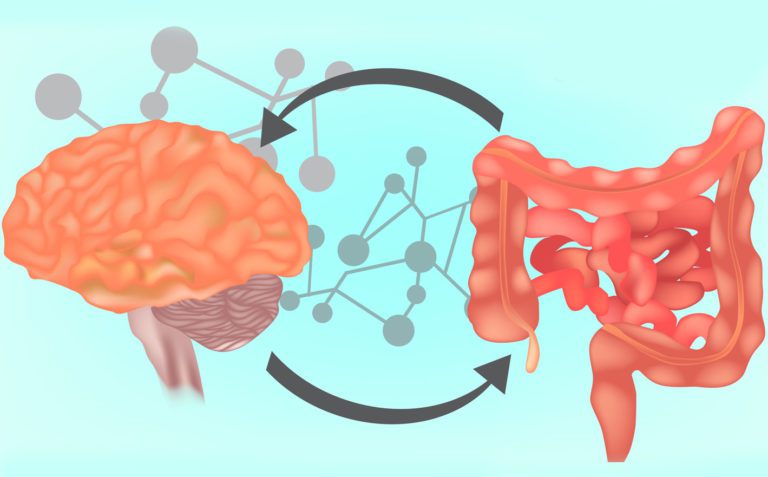
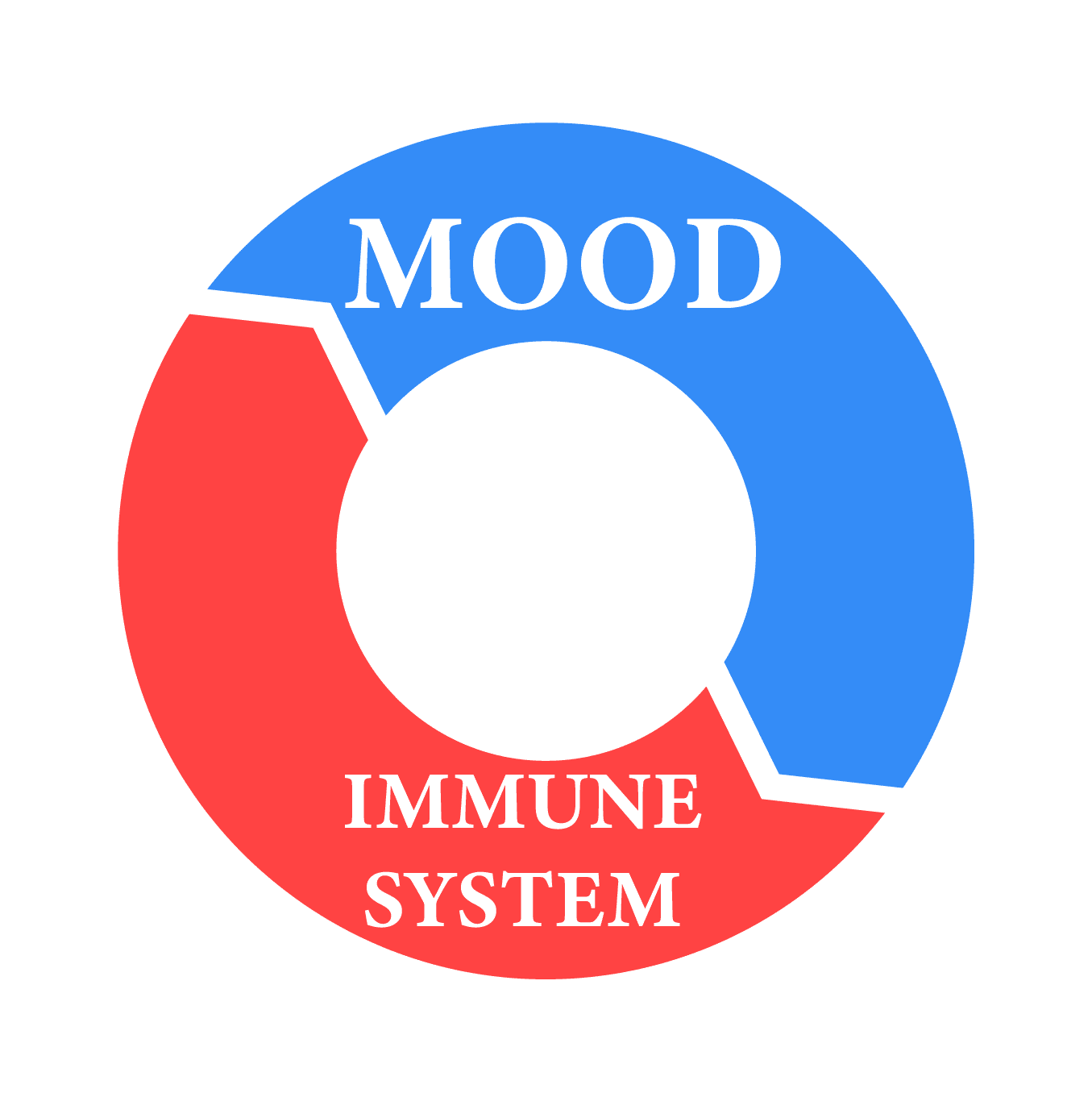
According to the science, it’s a two-way street. It’s not just ‘stress and immunity’. It’s also ‘immunity and stress‘. Chronic inflammation and a weak immune system can sabotage our mood, but conversely, stress can also drive up inflammation and leave our bodies vulnerable to microbial attack.
Our mood and our immune system strongly influence each other in the fashion of a feedback loop:
So what then are the biochemical mechanisms behind how stress can cripple the immune system?
There are numerous neuroimmune pathways that have been explored by researchers, but one of the most well-known ones has to do with an inflammatory transcription factor called NF-kB, which stands for ‘nuclear factor kappa-light-chain-enhancer of activated B cells’.
NF-kB is called a ‘transcription factor’ because it’s able to alter the way that DNA is transcribed. In this case, the DNA that it affects relates primarily to the control of inflammation and immune function.
NF-kB can be profoundly affected by stress, but is also activated by heavy metals, free radicals, and pathogens such as viruses and bacteria.
In fact, NF-kB is a virus’s best friend.
Many viruses have learned how to appropriate the NFkB pathway to evade your immune system and increase their replication within your cells. Inhibiting NF-kB is potentially an effective strategy in dealing with COVID-19.
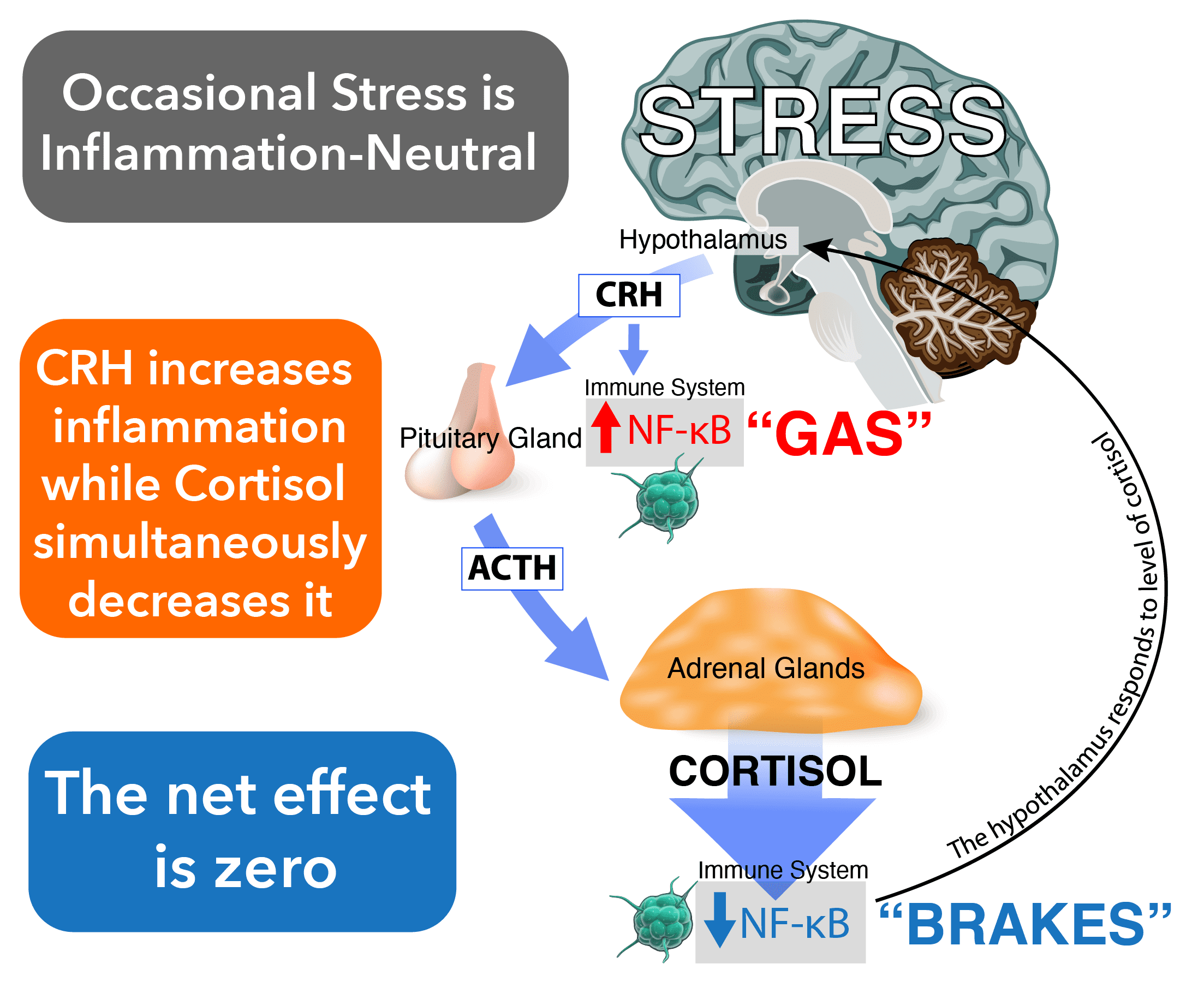
There’s a big difference between occasional isolated stress and chronic stress, however. First, let’s talk about how occasional stress is supposed to work, in a person who is generally healthy and has fairly little stress:
1 – Something stresses you out, whether it’s an actual imminent threat, such as almost getting in a wreck on the freeway, or just an unpleasant thought, such as worrying about your bills or your relationship.
2 – Your brain switches into stress mode, and your hypothalamus releases CRH (Corticotropin-releasing hormone).
3 – CRH travels the short distance from your hypothalamus to your pituitary gland, and your pituitary then produces ACTH (Adrenocorticotropic hormone). At the same time, it also tells your immune system to increase inflammation by making your macrophages create more NF-kB.
In other words, CRH hits the GAS on inflammation.
4 – The ACTH your pituitary gland just made then leaves the brain and travels through your blood until it hits the adrenal glands.
5 – Once that ACTH reaches your adrenal glands, they now produce cortisol, which decreases NF-kB and tells your hypothalamus to calm back down.
While CRH hit the GAS, cortisol hits the BRAKES on inflammation.
In this ‘perfect world’ scenario of occasional stress, the net effect should be zero.
It’s a well-designed feedback loop with a system of checks and balances that keeps inflammation in check. CRH increases NF-kB while cortisol decreases it.
Here’s another look at it:
Unfortunately, that’s not the reality that many of us live in, especially in the post-COVID era. People are stressed to the max. There are bills to be paid, marital fights to be had, and mountains of things to worry about.
We’re activating our stress chemistry on a regular basis. Many of us also live with trauma, which can dysregulate the hypothalamic-pituitary-adrenal (HPA) axis and negatively affect our inflammatory pathways.
Chronic stress is an entirely different animal, and it can have devastating consequences for the immune system.
According to the Glucocorticoid Resistance Model of stress, as stress becomes chronic, it starts becoming pro-inflammatory because our cortisol receptors become desensitized. When these receptors are no longer responsive, then cortisol can’t do its job of turning down NF-kB and shutting off inflammation.
Here’s that same diagram again, but showing what happens when with repeated activation of stress pathways:
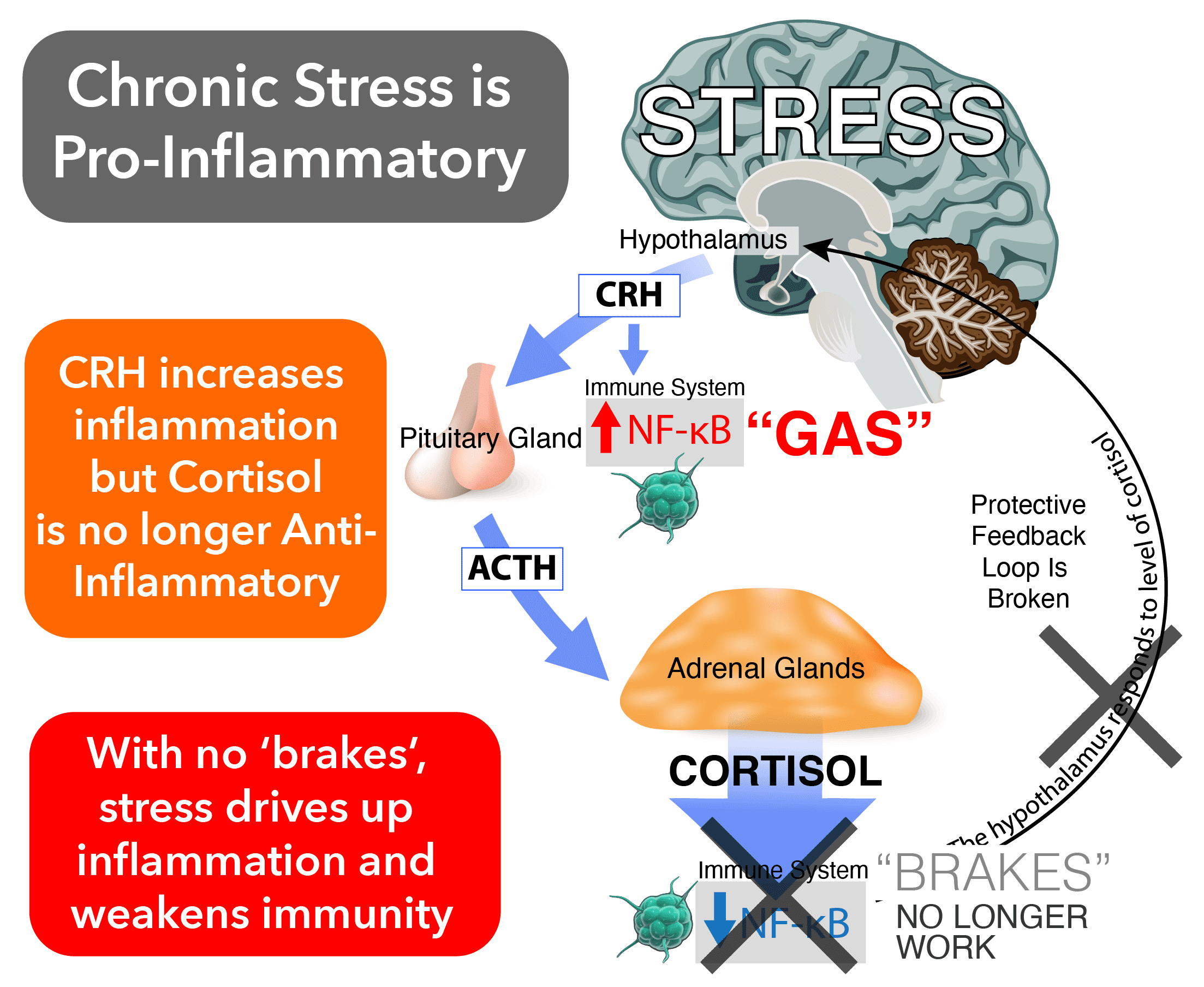
It should be noted that this is only one model of just how stress is able to drive up inflammation and weaken the immune system. Immunology is incredibly complex, and so anyone wanting a full explanation will have to dive much deeper into the research.
There are countless investigations into the connection between stress and immunity. We know, for example, that meditation, mindfulness, and even forest bathing can powerfully affect our quality of life by keeping the immune system balanced and unencumbered by the ravages of chronic inflammation.
We’re now at a point where mind-body medicine has become mainstream. It’s not just for your weird uncle who walks barefoot and only drinks water blessed by a shaman. This stuff is real, it’s immediate, and it’s more crucial to appreciate now than it ever has been.
A healthy lifestyle, with the right superfoods, adaptogenic herbs–and time set aside for exercise, positive social interaction, and mindful relaxation–is something which we should all strive to create for ourselves if we’re truly looking to prosper while the world only grows more chaotic every day.