“The map is not the territory.”
-Afred Korzybski
Humans love to oversimplify reality because it makes it infinitely easier to understand.
Because we specialize in metaphor-making, we tend to mistake our stories about reality for actual reality, and we’re rarely aware of the unconscious reasons why we pick certain metaphors over others in the first place.
For example, we visualize electrons as a kind of cloud that hovers around the nucleus, when quantum reality is far, far more bizarre than we could ever rationally apprehend, and we can be fairly certain that there is no such thing as an electron “cloud”.
And of course there’s the missing heritability problem in molecular biology: the cold, hard reality that there are still massive gaps in our ability to explain all the traits of organisms based on their genetic code, something which defies the common notion that we have our own biology totally figured out.
We do not.
So then, considering our penchant for oversimplification and routinely confusing the map with the territory, it’s not surprising that we’ve done that with depression.
Given that over sixteen million US adults suffer from this often debilitating disease, it’s time that medical practitioners and laypeople alike grant it its due complexity and begin to acknowledge just how much we still don’t know about it.
Contrary to popular belief, depression is absolutely not explained by the ‘chemical imbalance’ theory, and it has potentially dozens of causes rather than merely one.
A few weeks ago, I did a deep dive into how the chemical imbalance hypothesis is now falling out of favor among professionals because the evidence behind it is shockingly anemic.
That article clearly struck a nerve with our readers, and considering how many of us are still under the spell of the tragically oversimplified chemical imbalance concept, it’s not surprising.
From the pandemic, to the riots, to financial insecurity, to rampant political divisiveness and the emotional fallout from social distancing, it’s an unbelievably stressful time to be alive, so it’s not a shock that depression has tripled since COVID hit.
With mood disorders and social isolation on the rise, it’s more important than ever to drop our illusions about how depression works and appreciate the multitude of causes it can have so that we can better understand how to treat it on a case-by-case basis that recognizes the uniqueness of each person.
Want to learn more about our top seller, CHOQ Purified Shilajit?
Check out our Shilajit Benefits page.
Deep Causes of Depression
A deep cause (AKA true cause) is something that originates from outside the body and could be considered a prime mover, meaning that by itself it can either cause or contribute to depression.
Some examples of deep (true) causes include:
- Nutrient Deficiencies
- Consumption of Gluten and Dairy
- Exposure to Mercury and Lead
- Exposure to Pesticides
- Trauma (especially during childhood)
- Alcohol Abuse
- Loss of a Loved One
- Social Isolation
- Epstein-Barr and other HHV family viruses
- Prescription Medications
(this is by no means an exhaustive list)
Note that ‘genes’ is not on this list for good reason. There is currently very little evidence that genes cause depression, despite the hollow pop psychology ‘wisdom’ that so many of us have been subjected to, which is merely an offshoot of the fallacious ‘broken brain’ narrative. Instead, genes would be an intermediate cause (which we’ll get to in a moment).
Certain genes are implicated in depression, but not in the sense that they directly cause it.
The APOE4 gene is associated with a 15x increase in the prevalence of Alzheimer’s disease because it reduces a person’s ability to remove mercury from the brain, and mercury can directly cause Alzheimer’s according to the research of biochemist Boyd Haley, PhD (read my article on that topic here if you’d like to learn more).
This gene is also associated with a higher risk of depression, which makes sense given that mercury is notorious for causing mood disorders. Still, this gene no more gives you depression than not wearing a seatbelt makes you get in a car wreck. It simply enhances susceptibility to a true cause of the disorder (mercury).
Depression does cluster in families, but genes are not the only things we inherit from our parents. Keep in mind that viruses, bacteria, and heavy metals are all heritable, and that trauma, neglect, and addictions are unfortunately passed on from generation to generation behaviorally and epigenetically.
Intermediate (pseudo) Causes of Depression
As opposed to a deep cause, an intermediate cause (AKA pseudo-cause) is something that begins within the body, which is almost always itself the result of something that originated from outside of the body.
They aren’t true causes because they did not actually initiate the process. They are merely cogs in the machine. That being said, it’s still critical to our understanding of the pathophysiology and treatment of depression to understand these intermediate causes.
A few examples of intermediate causes include:
- Chronic Inflammation
- Thyroid disorders
- Poor Mitochondrial Function
- Hypoglycemia (low blood sugar)
- Genes (such as the aforementioned APOE4 gene)
- Neurotransmitter Deficiencies (although the evidence for this is shaky, they clearly play a role in mood regulation)
Again, the reason why these are intermediate causes rather than deep causes is that they’re describing processes in the body, rather than an independent, external influence.
So, anytime you’re contemplating an intermediate cause like ‘low serotonin’, the first question should always be: “what’s the underlying deep cause?” If someone has ‘low serotonin’, how did it get so low in the first place?
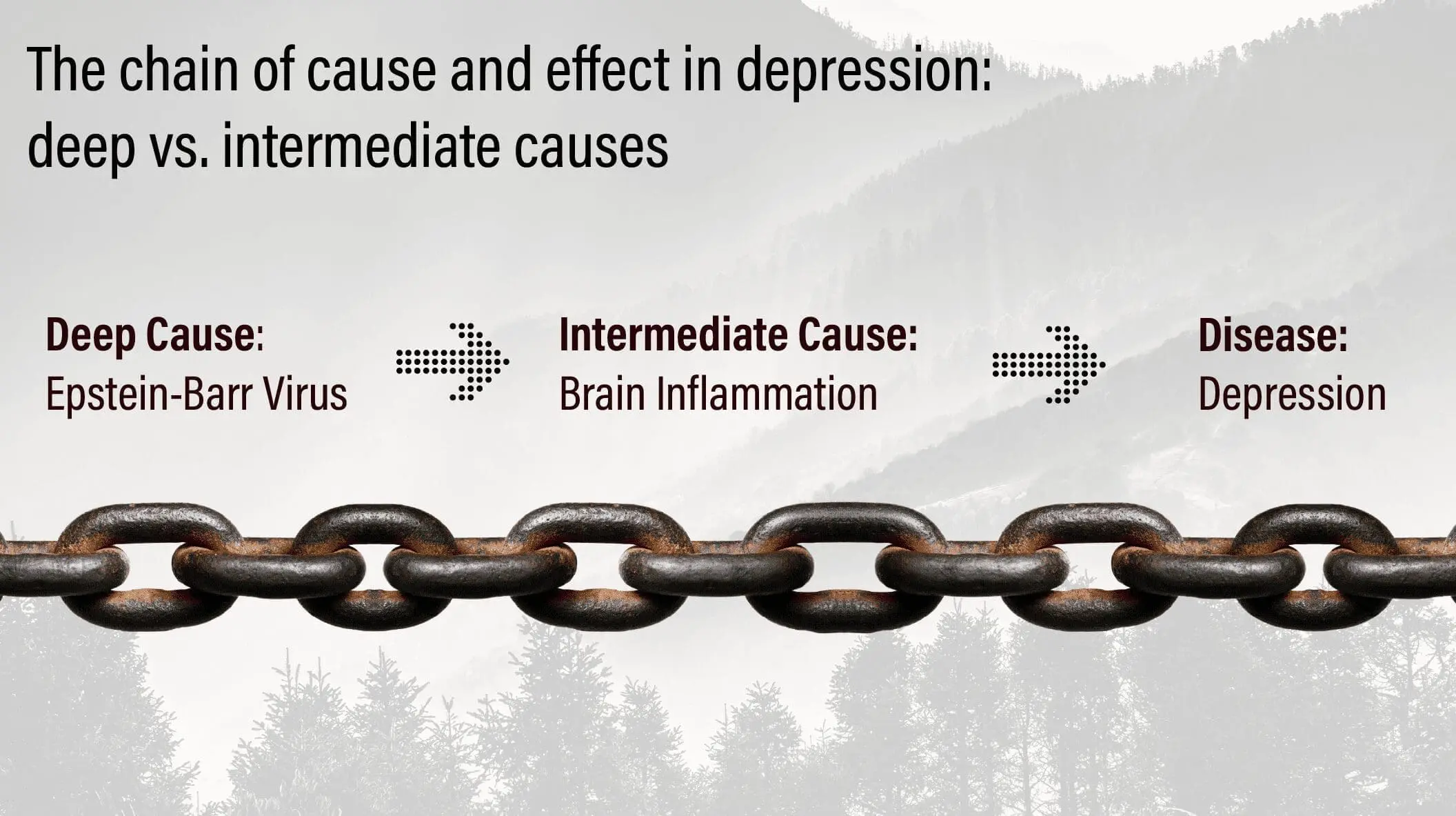
There’s a chain of cause and effect. Often, what we think of as a cause is merely one link in the chain.
Here’s an example of what the chain of cause and effect might look like in someone who has viral depression:
Inflammation: the most important intermediate cause of depression to investigate
Regarding intermediate causes, the most interesting (and clinically relevant) of all of them is chronic inflammation.
Researchers refer to this concept as the ‘inflammatory cytokine model of depression’ (cytokines are the molecular messengers that the immune system uses to turn inflammation on and off).
Inflammation is increasingly at the forefront of nearly every major chronic disease, from diabetes, to autoimmune conditions, to arthritis. Some are even calling it the root of all disease, which of course is a partial truth at best, as there is always a deeper cause underlying the inflammation that must be examined.
It’s important that we not fall prey to that all-too-common critical error: the idea that it’s all the immune system’s fault. This is tantamount to victim-blaming, and it’s used as justification for the suppression of the immune system, a truly dangerous strategy that has no place in anything other than emergencies.
The immune system is not the perpetrator. It’s doing its best under extremely challenging conditions. Although the immune system technically produces inflammation, the reason for the inflammation can always be traced back to a pathogen, toxin, stressor, or other deep cause.
With those caveats out of the way, let’s take a look at some of the research connecting depression and inflammation.
Evidence for the role of inflammation in depression:
1. Multiple inflammatory cytokines, such as Interferon-Alpha (IFN-B), Tumor Necrosis Factor Alpha (TNFa), and Interleukin-2 (IL-2) all produce symptoms of depression when given to human volunteers, such as loss of interest in social activities, poor appetite, fatigue, and social isolation.
2. Depressed patients tend to have higher white blood cell (WBC) counts in some studies, suggesting an inflammatory response to a pathogen.
3. Interleukin 1 beta (IL-1B), another cytokine that turns on inflammation, has profound effects on both serotonin and stress hormone activity in the brain.
4. Patients being given anti-inflammatory drugs have reported significant improvements in symptoms of depression.
5. Many of the deep causes of depression, such as gluten, pathogens, and toxins, are all pro-inflammatory, suggesting that inflammation may be the universal link that applies in the vast majority of cases.
Impressive as those points are, they’re just the tip of the iceberg. The research goes far, far deeper.
If you’d like to explore further, I highly recommend Cytokines and Depression, which is available for free online and also on Kindle. It contains hundreds of references to studies like the ones above.
The maps of the future
If you’re suffering from depression and aren’t sure where to turn to, find an integrative medical practitioner who can help you develop a plan that addresses the deeper physical and mental causes that are relevant to your unique case while also making use of the best anti-inflammatory nutritional, herbal, and lifestyle strategies.
Know that stealth pathogens like EBV are one of the greatest deep causes of inflammation, and that—no matter what—you will want to support your immune system in as many ways as possible in order to get inflammation under control.
We’re on the precipice of a new paradigm of mental health, one in which gross oversimplifications will no longer be acceptable, and drive-through ‘McMedicine’ will be a thing of the past.
If you’re one of the people who’s waking up to the greater complexities of medicine, as well as the impact that pathogens, toxins, and a mismatch of biology and environment have on the human body, know that you’re helping to create the future of health and wellness, and that you’re doing the world a great service.
The map is not the territory, but we humans–who are steeped in language and metaphor and meaning–will always need maps. Let’s do our best to upgrade them so that they more accurately illustrate the real topography of the mind and body and truly serve those who are suffering.






