It seems that common sense is an increasingly rare commodity these days.
It’s true that the world is in a steady state of increasing complexification. Year after year, the way we do things becomes significantly more ‘new-fangled’, for lack of a better term. We love anything that smacks of technological progress, as our very economic wellbeing is predicated upon it.
We’re low-key victims of complexity bias. Ever heard of it? If we modern humans are fish, then this bias is the water we’re swimming in. It’s hard to see: invisibility through ubiquity.
Put simply, complexity bias is the human tendency to make tasks that should be extremely simple far more complex than they actually need to be. It’s complexity for complexity’s sake…a symptom of the highly synthetic and simulated world we humans have created for ourselves.
In other words, someone suffering from complexity bias might—instead of moving through a simple, linear 3-step process—prefer a vulgarly abstruse 17-step hokey pokey, complete with spreadsheets, flow charts, algorithms, and maybe even a half-time show. No doubt, this kind of thinking has its place, but it should be used only when actually necessary.
So why have I spent the first 200 words of an article about gluten sensitivity waxing philosophical about our obsession with complexity?
It might seem like a digression, but I assure you it’s not.
Modern medicine is the complexity fetish poster child, and one of the most profound demonstrations of its predilection for this unwieldy methodology is the way that the much of the medical community looks at gluten intolerance.
That isn’t to say that there aren’t a lot of complexities regarding the scientific investigation of gluten sensitivity and that these complexities should be oversimplified. We’ll get to that in a bit. But before we do, let me tell you a story that perfectly illustrates my point.
An Exercise in Diagnostic Futility
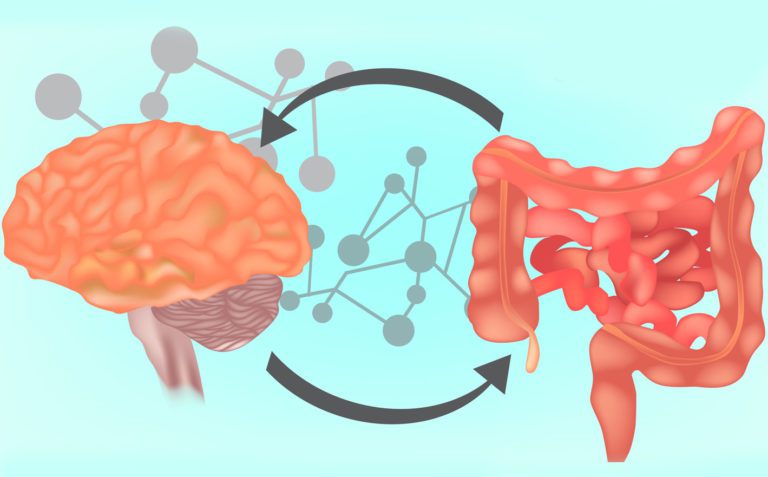
A few years ago, I had a client who had an 8-year-old son with a host of digestive and mood problems. Being aware of the mind-gut axis and how gluten causes these kinds of issues in certain people, she decided to put her son on a mostly gluten-free diet and found that there was a massive improvement in many of his symptoms.
Every time he ate a significant amount of wheat, his health suffered in numerous ways. It thus seemed reasonable to assume that this boy was gluten intolerant. In her mind, she had all the proof she needed.
When she spoke to a physician about it, however, she was told that the only way to know whether her son had issues with gluten was to test him for celiac disease and that the improvement of his symptoms was essentially meaningless because it was totally subjective.
In other words, he entirely dismissed her son’s direct experiences of gluten intolerance. Because she was not a doctor, her case report was irrelevant.
When she asked him what the testing process for celiac disease entailed, the physician informed her that her son would have to do the following:
- Go back on gluten for 6-8 weeks, potentially causing harm to his system and creating all manner of systemic inflammation leading to more digestive and behavioral problems (this is done in order to ensure that the bloodwork is accurate)
- Get bloodwork that would look for the presence of antibodies that indicate immunoreactivity to wheat proteins as well as the body’s ability to generate antibodies in general (tTG-IgA, EMA, and total serum IgA)
- Receive an endoscopy and small intestinal biopsy, a procedure in which he would go under general anesthesia and then have a tube inserted down his throat, all the way through the stomach and into the small intestine, and then have a tissue sample removed from the intestinal lining so it can be analyzed
[Want to make your brain hurt? Check out the actual flowchart that describes the Mayo Clinic’s official Celiac Disease diagnostic testing algorithm. It’s asininely complex.]
So what do you think the woman told the physician?
Let’s just say she gave him a hard no.
For months, this woman had watched her son’s symptoms improve dramatically after lowering gluten, and get massively worse every time he increased his consumption of it.
This physician wanted her to make her child suffer through 2 months of eating gluten despite clear indications that it was hurting him, then to pay in excess of a thousand dollars out of pocket for various blood tests and a biopsy of his small intestine. Then, and only then, would the physician take seriously the idea that this boy’s life might be better without gluten in it.
Complexity bias par excellence.
This physician was likely taught in medical school that if the aforementioned tests fail to confirm that a patient has celiac disease, then wheat can definitively do no harm to that patient.
Medical technologies like blood tests and biopsies are 100% objective and therefore tell the absolute truth. A patient’s direct experience of feeling different after making a dietary change doesn’t matter.
Such is the unmitigated hubris inherent in the modern medical model’s approach to food sensitivities.
Non-Celiac Gluten Sensitivity
Let’s say a woman speaks with a friend who saw a natural healthcare practitioner who convinced her to stop eating gluten, and that her friend now feels better, has less joint pain, and lost a little weight.
Perhaps she then decides to ask her doctor about whether it’s a good idea to stop eating gluten. Many physicians are still going by the outdated, binary, black-and-white model that says: either a patient has celiac disease and can’t have any gluten at all, or the patient does not and can eat as much as he or she likes.
In this model, there are no gray areas.
This means that there’s a high probability that the woman in this hypothetical situation would be told by her doctor that she must go through the customary rigamarole, including the bloodwork and the endoscopic biopsy, and if she’s negative then it’s pointless to cut wheat and other gluten-containing foods from her diet.
If she isn’t diagnosed with celiac, then she will assume that gluten is perfectly ok to eat and that there are no other methods by which she could evaluate whether it’s harmful to her.
Unbeknownst to far too many physicians, the reality of the situation is that there are many, many people who do not tolerate wheat but who also don’t meet the criteria for celiac disease. Many doctors are simply not up to date with the scientific literature on gluten sensitivity and don’t know the current technological limitations regarding how we measure the inflammatory effects of wheat.
Those doctors who are more current with the state of research on this topic would know, however, that there are plenty of folks who don’t have celiac disease but still cannot handle gluten.
There are two terms commonly in use for this condition. The first is Non-Celiac Gluten Sensitivity (NCGS) and the second is Non-Celiac Wheat Sensitivity (NCWS) (the reason being that there are various compounds in wheat other than gluten that may cause problems, for example FODMAPs and amylase-trypsin inhibitors).
Regardless of what you call it though, it’s very real, outdated medical school curriculums notwithstanding.
A 2019 systematic review of various studies on Non-Celiac Gluten Sensitivity had the following to say:
“The heterogeneous groups of patients affected by NCGS are composed of a number of subgroups, and each demonstrates different clinical and pathological manifestations. The presence of certain underlying factors can be utilized to identify susceptible individuals, namely, incidence of food allergies in infancy, anti-gliadin IgG-antibodies, activation test for flow cytometric basophils, atopy, and increased intraepithelial duodenal eosinophil presence. There is urgent need for reliable biomarkers to decisively diagnose and differentiate NCGS from related disorders.”
My translation:
“We still don’t really know exactly why so many people without celiac disease can’t handle eating wheat and other gluten-containing foods, but we do finally recognize that it’s a real problem, and we hope to figure out how to create lab tests that will accurately diagnose Non-Celiac Gluten Sensitivity in the future. Hold tight. We’re working on it.”
Is it Really All in Your Head?
When it comes to evaluating whether something is the result of the placebo effect, people are far more likely to invoke it when the intervention in question is something that they’re biased against.
For example, if you were to tell an older, more conventional physician that your depression was alleviated by taking herbal extracts, he or she might invoke the placebo effect explanation, but if you were to say that an SSRI is what got you better, then there would be no need to even go there (despite the fact that many antidepressants are barely more effective than placebo).
There have been several placebo-controlled studies on Non-Celiac Gluten Sensitivity, and many of them have found that, when gluten was added back into the diets of those who had abstained for a while, there were significant increases in symptoms in the groups who got the gluten versus placebo.
In a 2015 study with 72 IBS patients, gluten was removed for 6 weeks and symptoms were monitored for improvement. They were then split into two groups, one who received 100 grams per day of gluten flour, and another who got 100 grams of a mixture of rice flour, corn starch, and glucose. They consumed this daily for another 6 weeks.
The patients who received the gluten flour had significantly poorer stool consistency, as well as more tiredness, bloating, and nausea. One issue, however, is that the placebo control should have been far more inert. Rice and corn can also be problematic for some people (corn contains FODMAPs, which are compounds of concern for some people with IBS).
Another widely cited placebo-controlled study on NCGS is also problematic. The researchers were actually careless enough to use both corn and lactose in the placebo control flour.
What these people did is the equivalent of testing a new painkiller and then using aspirin as a placebo. That’s just poor experimental design, plain and simple. In their defense, they do point this out as a limitation of the study in the discussion section, but it would have been wiser just to find a more inert placebo control in the first place.
One-third of the participants in the study were still deemed to have NCGS, based on the way their symptoms increased when they were given gluten but not the placebo. The whole study only lasted a few weeks, however, so it’s hard to know how generalizable this is to real life, in which people eat gluten on a daily basis for decades.
And then there’s yet another problematic study in which the control was whey protein. Again, controls need to be as hypoallergenic as possible, which means dairy-free.
Want to See if Gluten is Hurting You? Do It the Old Fashioned Way.
Functional medicine practitioner Chris Kresser is known for saying the true gold standard for diagnosing whether or not you’re sensitive to wheat/gluten is simply eliminating all gluten-containing foods 100% for two months and then reintroducing them and monitoring your reaction.
I agree with Kresser wholeheartedly.
In my clinical experience, many people will immediately discover digestive and inflammatory symptoms upon reintroducing gluten, but there is a subset who will not notice until perhaps a few weeks. It may be necessary to continue the gluten challenge for a couple of weeks if your symptoms are slow to change.
If you don’t have any digestive issues, then you will have to track other symptoms, such as energy levels, mood, stress, focus, joint pain, etc.
It’s best to keep a symptom journal. If you’re dealing with something like acne, for example, you’ll want to take pictures and monitor your progress carefully. It’s also helpful to work with a nutritionally-informed integrative medical practitioner. A trained professional will know what to look for and can help you stay on track.
Sixty days gluten-free will be enough time for some symptoms to improve, but not others. Many issues are multifactorial, so simply eliminating one contributing factor that’s adding fuel to the fire of systemic inflammation may not always be enough to move the needle.
Also remember that, in order to be a good scientist, you need to only change one variable at a time.
In other words, if you really want to know whether going without gluten is helping your mood, then don’t also start taking huge doses of rhodiola or meditating daily at the same time you stop eating bread, because you won’t know what to attribute the positive effects to.
At the end of the day, though, here’s the most important thing to know: you’re allowed to trust your own experience when it comes to how things affect you when you put them in your body. Your perceptions are valid. Don’t let anyone convince you otherwise.
We’re all susceptible to the placebo effect, and the mind-body connection is indeed profoundly powerful. Unfortunately, we don’t all have the ability to design a perfect placebo-controlled study to find all of our food intolerances, and the various assay technologies that we have to diagnose these issues are clearly lacking, as too many people have fallen through the cracks.
Huge numbers of people claim that a vegan diet is what saved their health, while equally huge numbers of other folks say that it nearly killed them. What percentage of the effects that food has on us is based on our beliefs?
In the real world, there is no blinding, so we have to just live with the fact that sometimes our attitudes about certain foods can change how they affect us. That being said, there’s plenty of evidence that many people feel much better when they don’t eat gluten (especially those with digestive and autoimmune issues).
Is it all in their heads? For some of them, sure. But for millions of people with non-celiac gluten sensitivity, the positive effects of eliminating gluten have nothing to do with their beliefs. Rather, the scientific community has yet to discover all of the mechanisms of action by which wheat can wreak havoc on the body.
But you don’t have to wait for science to explain why you feel a certain way when you eat a certain food. Just because the ‘how’ hasn’t been fully explained, that doesn’t mean that your experiences of your own body aren’t real.